Advocacy
WPBDF serves people living with Hemophilia, von Willebrand Disease, and other rare bleeding disorders. Our service area includes 26 counties in Western PA. We provide education, advocacy, and many other services to help our members manage their disease and improve their quality of life.

We Represent You!
Advocacy is a key component of the Foundation’s mission. Our overarching goal is to preserve access to care for our community members in Pennsylvania. As such, we are involved with budgetary, policy and legislative issues that arise in Harrisburg. We are strategically positioned to be proactive in our advocacy efforts, while also being nimble enough to react when needed.
Under the leadership of both the Western and Eastern PA Bleeding Disorders Foundations, a coalition was formed that includes the seven HTCs in the state, the National Hemophilia Foundation, the Hemophilia Federation of America, and Milliron & Goodman Government Relations. This collaborative group is proud to represent You!
We frequently have meetings with the Department of Health, The Department of Human Services, the Insurance Commissioner’s Office and the Governor’s Office. In addition, we have developed strong relationships with legislative offices in both the PA House and Senate. We also get proclamations and resolutions adopted to recognize Bleeding Disorders Awareness Month in March and World Hemophilia Day on April 17. Buildings and landmarks are lit in red across the state of PA. This is extremely rewarding work that benefits the entire bleeding disorders community.
Understanding Federal Issues
Marketplace Updates for Open Enrollment
Big changes are coming this Fall to the ACA health insurance Marketplaces. New federal regulations, combined with the “One Big Beautiful Bill Act” signed into law on July 4th, mean that many insurance purchasers will face higher costs, new restrictions on eligibility, and more paperwork during open enrollment and beyond.
Helpful Resources:
- Click here to sign up for our action alerts.
- Action alert, Call on Congress to Keep the Health Care Tax Credit!
- Legislative Leave-Behind: Protect Americans with Bleeding Disorders - Extend the Enhanced Premium Tax Credit
- Slides from National BDC session, Decoding Your Insurance
- NBDF Insurance Toolkit
- Preparing for Marketplace Open Enrollment
- NBDF Webinar - Navigating Open Enrollment for Private Insurance this Fall
- Medicare in 2026
- Medicare in 2026 Q&A
Medicaid Updates
On July 4, 2025, President Trump signed into law a bill (the “One Big Beautiful Bill Act”) that cuts $1 trillion from the Medicaid program and makes sweeping changes to eligibility, enrollment processes, and more. You can see the One Big Beautiful Bill Act Timeline here.
Helpful Resources:
- Preparing for Medicaid Changes
- The One Big Beautiful Bill Act Timeline
- What Congress Latest Healthcare Cuts Mean for PA
- Q&A: What Congress’ Latest Healthcare Cuts Mean for Pennsylvania
PA Bleeding Disorders Stakeholders Meet to Collaborate

On December 2nd, the Western and Eastern PA Bleeding Disorders Foundations brought together HTCs, staff, and key partners for a statewide meeting. Participants shared ideas, reviewed policy updates, and explored ways to strengthen support and outreach for the bleeding disorders community.
Presentations from the meeting are listed below.
- Stakeholder Meeting 2025
- BDSUMHAC Update 2025
- NBDF - Federal Update 2025
- Milliron Goodman - State Update 2025
- PHLP - Understanding Medicaid Changes Ahead - December 2025

Understand the State Issues
As work continues on the FY 2025-26 budget process, we respectfully make the following requests:
- Increase state support from $1,017,000 to $1,250,000;
- Include language in the fiscal code to maintain the existing distribution of funding to the HTCs; and
- Maintain the hemophilia line item as a separate line item in the budget bill.
Hemophilia Line Item:
There are approximately 20,000 patients with hemophilia and thousands more with other inherited bleeding disorders in the U.S. More than 3,000 patients receive care in Pennsylvania at the HTCs, all of which have been recognized as centers of excellence by the Commonwealth.
The HTCs are critical to the patients who receive care at these facilities. Without this support, Pennsylvania will incur approximately 5x more costs for these citizens, from emergency and inappropriate care via Medicaid and lost tax revenue from those who become unable to remain gainfully employed. The Hemophilia Program saves Pennsylvania lives and saves Pennsylvania money.
The line-item funding goes to each of the seven hemophilia treatment centers (HTCs) for direct patient care, not research. HTCs provide comprehensive care via specially trained multi-disciplinary teams that include hematologists, pediatricians, nurses, social workers, and physical therapists, among other healthcare providers and services. Studies conducted by the Center for Disease Control (CDC) demonstrate a 40% reduction in mortality and medical complications in patients who receive their care at an HTC compared with those followed by hematologists outside of this network. The overall costs of care are reduced as well, providing an excellent return on investment.
It is important to note that 100% of the Hemophilia Program line item goes directly to patient care (i.e., mostly for non-billable nursing and social work services vital for patient care). A portion is also used as an emergency fund to help patients in financial hardship due to their bleeding disorder. For the past few years, there have been an unprecedented number of requests.
As an example, the Hemophilia Center of Western PA received $204,406 for the 2024-25 fiscal year and they utilized these dollars for some of the following initiatives:
- Supporting patients with transportation costs, allowing patients to attend necessary appointments. They have also been vital for accessing rare medications that are often costly and inadequately covered by insurance;
- Supporting routine screenings for conditions like anxiety, depression, and PTSD are critical for identifying and addressing behavioral health issues that often accompany chronic illnesses. While these screenings are conducted regularly, the significant shortage of providers who accept Medical Assistance complicates timely access to care for our most vulnerable patients. The funding helps facilitate referrals and overcome some of these systemic barriers, although the need for expanded resources remains urgent;
- Supporting the Unified Care Protocol (UCP), a transformative framework aimed at eliminating barriers to care and improving health outcomes for patients. The UCP is essential for developing a comprehensive, patient-centered approach that acknowledges
the complexities involved in managing bleeding disorders. It not only focuses on medical treatments but also emphasizes the vital need for psychosocial support and assistance in navigating healthcare systems. By ensuring that everyone receives holistic care tailored to their unique circumstances, the UCP significantly enhances the quality of life for patients of all ages and backgrounds; and - Supporting the Consumer Advocacy Council, which convenes three times a year to provide a platform for patients and families to voice their concerns and suggestions;
In 2022, we were pleased to receive a 6% increase to the Hemophilia line item in state budget from $959,000 to $1,017,000 and language in the fiscal code to ensure these funds are distributed to all 7 Hemophilia Treatment Centers in Pennsylvania. Each year, we must continue our work to maintain this funding.
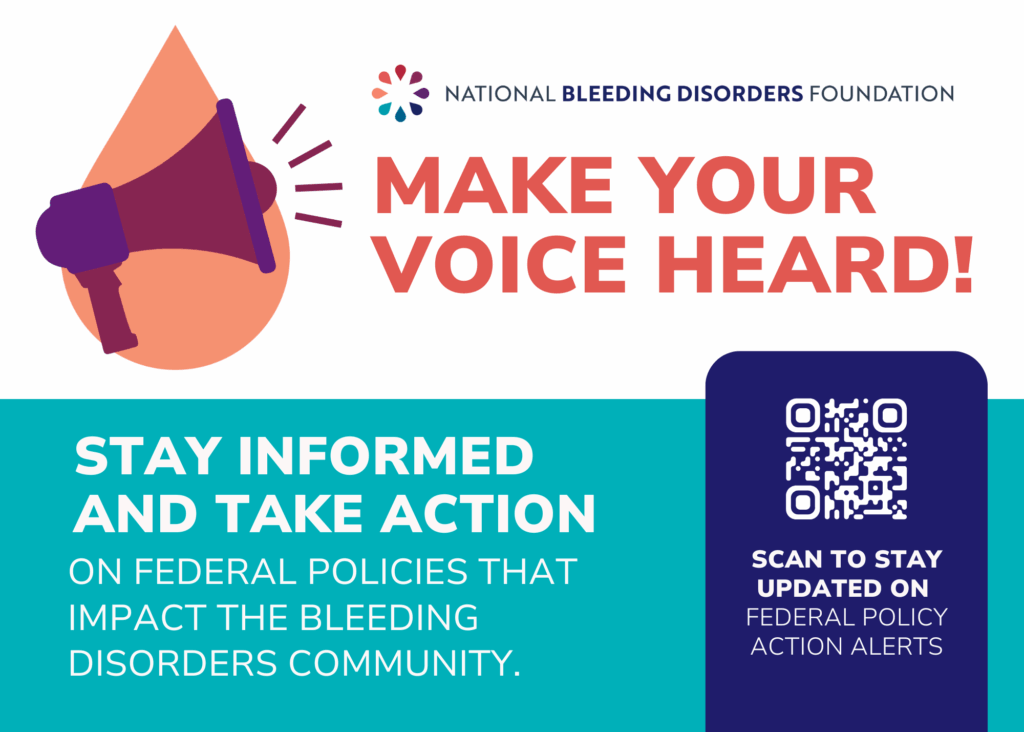
Copay Accumulators, Maximizers, and Alternative Funding/Specialty Drug Carve Outs
Many individuals with bleeding disorders rely on copay assistance to access their high-cost medication. Over the past several years, many Pennsylvanians have had insurance companies institute copay accumulator and maximizer programs on federally regulated plans. This does not allow copay assistance to count toward deductibles or out-of-pocket maximums, as it traditionally has. Copay accumulator programs allow health insurers and pharmacy benefit managers to take the benefit of the copay assistance rather than passing it on to consumers, as it was intended. We want to be proactive and ensure this does not occur in marketplace and state regulated plans.
Learn more about copay accumulators, maximizers, and alternative funding:
- Copay Accumulators Patient Impact Video
- Voices for Policy Change
- Slides: Alternative Funding schemes: What are they and what CAN WE DO TO STOP them?
- Feature on Copay Accumulator Assistance with WTAE-TV Pittsburgh
Ask State Senators to support SB 268, to proactively protect Pennsylvanians in state-regulated health plans by clarifying that all payments made by the patient or on behalf of the patient count toward the patient’s deductible and OOP costs.
- SB 268 (Ward, R-Blair): Amends the Insurance Company Law by requiring insurers to count the drug manufacturers’ assistance program towards the deductible and out-of-pocket costs.
- The bill was introduced and referred to the Senate Banking & Insurance Committee, where it currently waits for consideration.
Ask State Representatives to support a companion bill in the House to proactively protect Pennsylvanians in state-regulated health plans by clarifying that all payments made by the patient or on behalf of the patient count toward the patient’s deductible and OOP costs.
Remember, you are your own best advocate. Let your voice be heard.
If you have any questions, would like to become an Advocacy Ambassador, or would like additional materials or information, please contact Kara Dornish, Executive Director at kara@wpbdf.org or 724-741-6160.